Introduction
Contraceptive devices are specialized medical tools or appliances designed to prevent conception, thereby enabling individuals and couples to regulate fertility and control reproduction according to their personal, social, and economic needs. These devices form a vital component of family planning, reproductive health, and population control programs worldwide.
Contraception, in the broader sense, aims to interrupt one or more stages in the reproductive process—from ovulation and fertilization to implantation of the fertilized egg—without interfering with the normal physiology of sexual intercourse. The development and use of contraceptive devices have had profound implications on public health, reducing maternal mortality, preventing unwanted pregnancies, and empowering individuals—especially women—to make informed choices about their reproductive lives.
In modern medicine, contraceptive devices vary widely in design, mechanism, and duration of action. They can act locally (e.g., condoms, IUDs) or systemically (e.g., hormonal implants and injectables). Understanding their structure, function, and physiological effects is essential for effective, safe, and rational use.
Classification of Contraceptive Devices
Contraceptive devices can be classified based on their mode of action, method of application, and duration of effectiveness. The major categories include:
- Barrier Methods
- Intrauterine Devices (IUDs)
- Hormonal Contraceptive Devices
- Permanent (Surgical) Methods
- Emergency Contraceptive Devices
1. Barrier Methods
Barrier methods work by physically blocking the entry of sperm into the female reproductive tract, thereby preventing the meeting of sperm and ovum. These are among the oldest and most commonly used contraceptive methods, dating back to ancient civilizations.
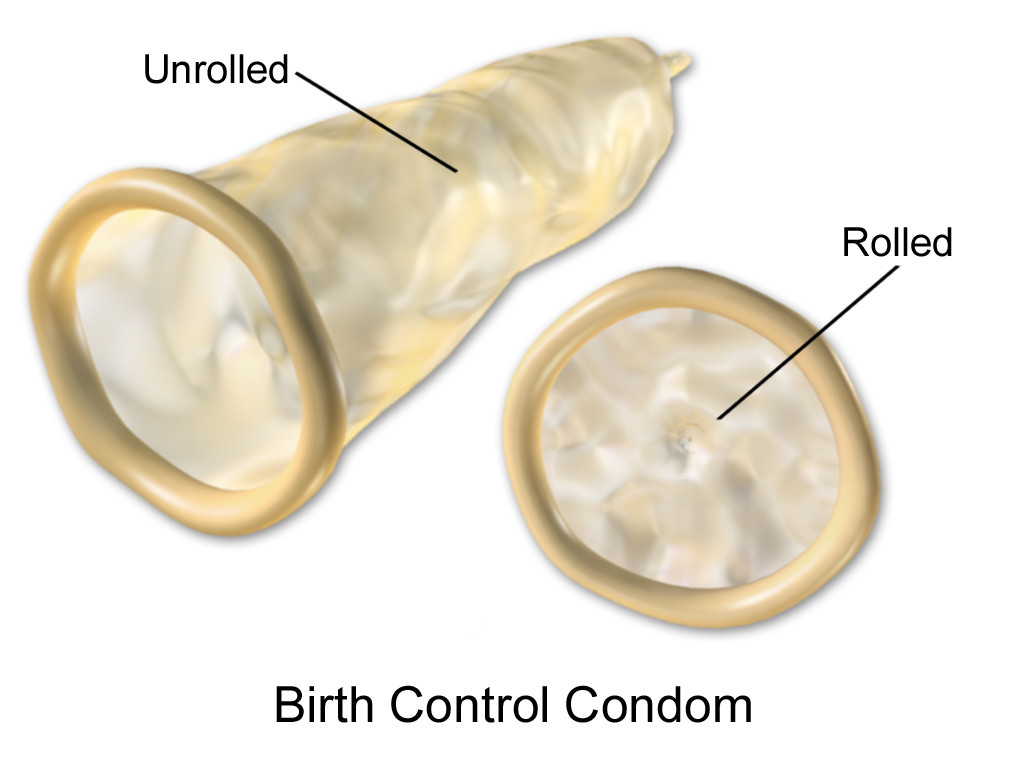
a) Male Condom
A male condom is a thin, flexible sheath made from materials such as latex, polyurethane, or polyisoprene, designed to be worn over the penis during sexual intercourse. Its primary purpose is to act as a contraceptive device, preventing the entry of sperm into the vagina and thereby reducing the risk of unintended pregnancy. Additionally, it serves as a protective barrier against sexually transmitted infections (STIs), including HIV, gonorrhea, and chlamydia.
Mechanism:
The male condom functions as a mechanical barrier. By covering the penis, it prevents semen from entering the vagina, which effectively stops fertilization. Simultaneously, it forms a barrier against infectious agents, thereby reducing the transmission of sexually transmitted infections. Unlike hormonal contraceptives, condoms provide protection without altering natural hormonal balance.
How to Use:
- Check the packaging and expiry date to ensure the condom is safe to use.
- Open the package carefully, avoiding sharp objects, fingernails, or teeth that may tear the condom.
- Pinch the tip to leave space for semen collection.
- Roll the condom onto the erect penis before any genital contact.
- After ejaculation, hold the base of the condom while withdrawing to prevent it from slipping off.
- Dispose of it safely in a trash bin; never reuse or flush condoms.
- Use water-based or silicone-based lubricants with latex condoms, as oil-based products can weaken the material and increase the risk of breakage.
Effectiveness:
- With typical use, condoms are about 85% effective, often due to inconsistent or incorrect use.
- With perfect use, meaning correct usage every time, their effectiveness rises to over 98%.
Advantages:
- Non-hormonal, so there are no systemic side effects.
- Provides dual protection against pregnancy and most STIs.
- Easily accessible, affordable, and widely available.
- Simple to use and reversible.
- No medical prescription is required.
Disadvantages:
- May slightly reduce sexual sensitivity or pleasure for some individuals.
- Risk of breakage or slippage if not used correctly.
- Some people may have latex allergies; alternatives are available but can be costlier.
- Effectiveness depends entirely on correct and consistent use; misuse can significantly reduce contraceptive efficacy.
b) Female Condom
A female condom is a soft, loose-fitting sheath made from materials such as polyurethane or nitrile that is inserted into the vagina before sexual intercourse. It serves as a barrier contraceptive, preventing sperm from entering the uterus, and provides protection against sexually transmitted infections (STIs), including HIV, gonorrhea, and chlamydia. Unlike male condoms, it is worn internally by the woman.

Mechanism:
The female condom works as a mechanical barrier, lining the inside of the vagina and covering part of the external genitalia. By preventing sperm from reaching the cervix, it reduces the risk of pregnancy. Simultaneously, it acts as a barrier against pathogens, lowering the risk of STIs.
How to Use:
- Check the package and expiry date to ensure the condom is safe to use.
- Open carefully, avoiding sharp objects that could tear it.
- Find a comfortable position (standing with one leg raised, squatting, or lying down).
- Squeeze the inner ring at the closed end and insert it into the vagina, pushing it up toward the cervix.
- The outer ring remains outside the vagina, covering part of the vulva.
- Guide the penis into the condom during intercourse to ensure it does not slip between the condom and the vaginal wall.
- After intercourse, twist the outer ring to seal in fluids and gently pull out.
- Dispose of it safely in a trash bin; do not reuse or flush.
Effectiveness:
- With typical use, female condoms are about 79–95% effective in preventing pregnancy.
- With perfect use, their effectiveness rises to over 95%.
- Effectiveness can be reduced if the condom is inserted incorrectly or slips during intercourse.
Advantages:
- Provides dual protection against pregnancy and STIs.
- Can be inserted before sexual activity, allowing more spontaneity.
- Non-hormonal and reversible.
- Useful for women whose partners cannot or will not use male condoms.
- Can increase a woman’s control over her sexual health.
Disadvantages:
- Slightly more expensive and less widely available than male condoms.
- Some individuals may find insertion awkward or uncomfortable at first.
- Can slip or bunch up if not inserted correctly.
- May make a slight noise during intercourse, which can be distracting for some.
c) Diaphragm and Cervical Cap
A diaphragm is a shallow, dome-shaped, flexible cup made of silicone or latex that is inserted into the vagina to cover the cervix. It acts as a barrier contraceptive, preventing sperm from entering the uterus and thereby reducing the risk of pregnancy. Diaphragms are typically used with a spermicide to increase effectiveness.

Mechanism:
The diaphragm works by physically blocking sperm from entering the cervical canal. When used with a spermicide, it immobilizes or kills sperm on contact, further reducing the likelihood of fertilization. Unlike hormonal methods, it does not affect a woman’s hormonal balance.
How to Use:
- Apply a small amount of spermicide to the inner surface of the diaphragm before insertion.
- Fold the diaphragm and insert it into the vagina, pushing it up to cover the cervix completely.
- Ensure the diaphragm fits snugly over the cervix; it should stay in place during intercourse.
- Leave the diaphragm in place for at least 6–8 hours after intercourse, but not more than 24 hours.
- Remove, wash with mild soap and water, and store in a clean, dry place.
Effectiveness:
- With typical use: ~88% effective.
- With perfect use: >94% effective.
- Effectiveness increases when combined with spermicide.
Advantages:
- Non-hormonal and reversible.
- Can be inserted hours before intercourse, allowing spontaneity.
- Provides partial protection against certain STIs (mainly those transmitted via genital contact).
Disadvantages:
- Requires proper fitting by a healthcare provider.
- Must be used with spermicide for maximum effectiveness.
- Risk of urinary tract infections or vaginal irritation in some women.
- May be cumbersome to insert or remove initially.
Cervical Cap
A cervical cap is a small, thimble-shaped silicone or latex device that fits tightly over the cervix to prevent sperm from entering the uterus. It is a barrier contraceptive often used with spermicide. Cervical caps are smaller than diaphragms and provide contraception for women who may not tolerate diaphragms well.
Mechanism:
The cervical cap physically covers the cervix, blocking sperm passage into the uterus. Spermicide used with the cap immobilizes or kills sperm, enhancing contraceptive effectiveness. Like the diaphragm, it is non-hormonal and does not affect ovulation.
How to Use:
- Apply spermicide to the inside of the cap before insertion.
- Insert the cap into the vagina, ensuring it fits snugly over the cervix.
- Leave in place for at least 6 hours after intercourse, but no longer than 48 hours.
- Remove, wash, and store as per instructions.
Effectiveness:
- With typical use: ~71–86% effective.
- With perfect use: ~86–96% effective.
- More effective in women who have never given birth vaginally.
Advantages:
- Non-hormonal and reversible.
- Can be inserted hours before intercourse.
- Small and discreet.
Disadvantages:
- Requires correct fitting by a healthcare professional.
- Less effective in women who have given birth vaginally.
- May cause vaginal irritation or urinary tract infections.
- Requires spermicide for optimal effectiveness.
d) Spermicides
Spermicides are chemical agents designed to kill or immobilize sperm, thereby preventing them from reaching and fertilizing an egg. They are used as a form of barrier contraception and are often applied inside the vagina before sexual intercourse. Spermicides are available in various forms, including gels, creams, foams, films, and suppositories.

Mechanism:
Spermicides work primarily by disrupting the cell membrane of sperm, immobilizing or destroying them on contact. When used with barrier methods, such as condoms, diaphragms, or cervical caps, spermicides enhance contraceptive effectiveness by reducing the number of viable sperm that can reach the cervix.
Forms of Spermicides:
- Gels and Creams – Inserted into the vagina using an applicator; provide immediate protection.
- Foams – Expand and coat the vaginal walls; easy to use but less effective than gels.
- Suppositories – Solid forms that melt at body temperature; inserted 10–15 minutes before intercourse.
- Film – Thin sheets placed near the cervix; dissolve quickly to release spermicide.
How to Use:
- Wash hands thoroughly before application.
- Insert the spermicide deep into the vagina, near the cervix, using the provided applicator or by hand (depending on the form).
- Most spermicides need to be inserted 5–15 minutes before intercourse for maximum effectiveness.
- If multiple acts of intercourse occur, additional spermicide may be required.
Advantages:
- Non-hormonal and safe for most women.
- Can be used on demand, without ongoing preparation.
- Often available over-the-counter without a prescription.
- Can be combined with barrier methods for enhanced protection.
Disadvantages:
- Less effective when used alone compared to other contraceptive methods.
- May cause vaginal irritation, burning, or allergic reactions in some users.
- Must be applied correctly and each time before intercourse.
- Cannot protect against all sexually transmitted infections, especially HIV.
Spermicides are best used as a complementary contraceptive method rather than the sole method due to lower effectiveness when used alone.
2. Intrauterine Devices (IUDs)
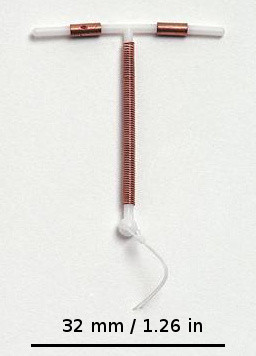
Intrauterine devices are small, T-shaped, or loop-shaped appliances inserted into the uterus by a trained healthcare provider. They provide long-term, reversible contraception and are among the most effective non-surgical methods available.
Types of IUDs
a) Non-Medicated (Inert) IUDs
Non-Medicated (Inert) IUDs are contraceptive devices made of plastic or other inert materials that are placed in the uterus to prevent pregnancy. Unlike copper or hormonal IUDs, they do not release any active substances, and their contraceptive effect is primarily due to the mechanical presence of the device. The device induces a mild inflammatory reaction in the uterus, creating an environment that is hostile to sperm and ova, thereby preventing fertilization. Inert IUDs are inserted by a trained healthcare professional, usually during menstruation, and a string is left protruding for self-check of placement. They are long-acting and reversible, typically effective for 5–10 years, but are slightly less effective than copper or hormonal IUDs. Advantages include being non-hormonal, having minimal systemic side effects, and requiring little maintenance, while disadvantages may include irregular bleeding, cramping, risk of expulsion, and no protection against sexually transmitted infections.
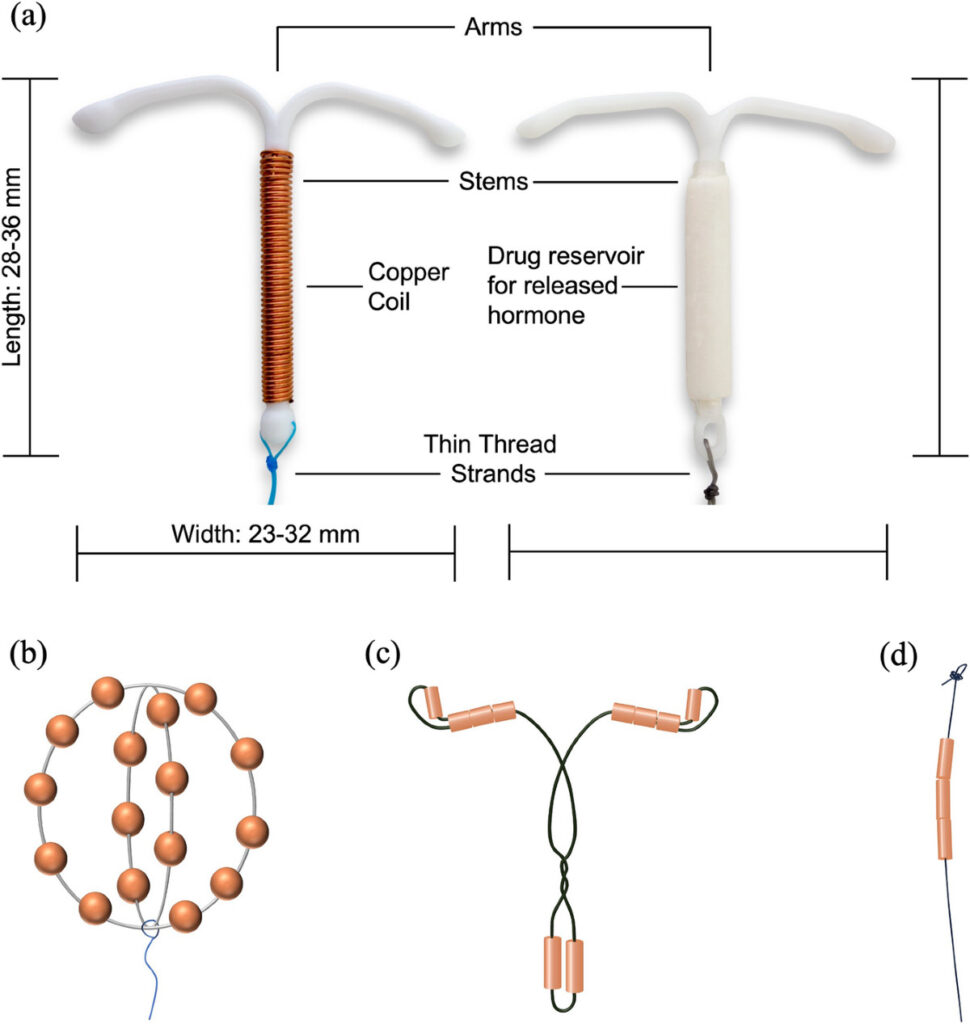
b) Copper-Releasing IUDs
Copper-Releasing IUDs are small, T-shaped intrauterine devices made of plastic and wrapped with copper wire, which are inserted into the uterus to provide long-term contraception. They are non-hormonal and prevent pregnancy primarily through the action of copper ions, which are toxic to sperm, reducing sperm motility and viability, and creating a uterine environment that is hostile to fertilization. Copper IUDs are inserted by a trained healthcare professional, typically during menstruation, and a string is left protruding into the vagina for self-checking placement. These devices are highly effective, with a failure rate of less than 1%, and can remain in place for 10–12 years depending on the type. Advantages include long-term, reversible, hormone-free contraception, while disadvantages may include heavier menstrual bleeding, increased cramping, and no protection against sexually transmitted infections.
c) Hormone-Releasing IUDs
Hormone-Releasing IUDs are T-shaped intrauterine devices that release a small amount of the hormone levonorgestrel directly into the uterus to prevent pregnancy. They work by thickening cervical mucus to block sperm, thinning the endometrial lining to prevent implantation, and sometimes partially suppressing ovulation. Hormonal IUDs are inserted by a trained healthcare professional, usually during menstruation, and a string is left in the vagina for self-checking. They are highly effective, with a failure rate of less than 1%, and provide long-term contraception for 3–7 years depending on the brand. Additional benefits include reduced menstrual bleeding and cramps, while disadvantages may include irregular bleeding initially, hormonal side effects in some users, and no protection against sexually transmitted infections.

3. Hormonal Contraceptive Devices
Hormonal contraceptives act by modifying the body’s endocrine functions, primarily by preventing ovulation and altering cervical and uterine environments to prevent fertilization or implantation. These methods are highly reliable when used correctly.
a) Oral Contraceptive Pills (OCPs)
Types:
Combined Pills: These contain both estrogen and progestin, the two primary female sex hormones. They are the most commonly used form of OCPs and are effective in preventing ovulation.
Mini Pills: These contain only progestin and are often recommended for women who cannot take estrogen, such as those who are breastfeeding or have certain health conditions.

Mechanism of Action:
- Suppression of Ovulation: OCPs inhibit the secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary gland, which prevents the maturation and release of the egg from the ovary.
- Thickening of Cervical Mucus: Progestin in the pills increases the viscosity of cervical mucus, making it more difficult for sperm to penetrate and reach the egg.
- Endometrial Alteration: OCPs cause changes in the uterine lining (endometrium), making it less receptive to implantation of a fertilized egg
Advantages:
- Regulation of Menstrual Cycles: OCPs help in maintaining regular periods and can significantly reduce the severity of menstrual cramps (dysmenorrhea).
- Reduction in Cancer Risk: Long-term use has been associated with a decreased risk of ovarian and endometrial cancers.
- Improvement in Acne and Hormonal Disorders: OCPs can reduce androgen levels, improving acne and other menstrual irregularities such as heavy bleeding or premenstrual syndrome.
- Other Benefits: They may also help with symptoms of polycystic ovarian syndrome (PCOS) and prevent ovarian cyst formation.
Disadvantages / Side Effects:
- Minor Side Effects: Some women may experience nausea, bloating, breast tenderness, weight gain, or mood changes.
- Cardiovascular Concerns: Rarely, OCPs may contribute to mild hypertension or increased risk of blood clots, especially in smokers or women over 35.
- Compliance Requirement: Daily intake is essential; missing doses can reduce effectiveness and increase the risk of unintended pregnancy.
- Other Considerations: Not suitable for women with certain conditions like a history of thromboembolism, liver disease, or estrogen-sensitive cancers.
b) Injectable Contraceptives
Examples:
Depo-Provera (Medroxyprogesterone acetate): One of the most widely used progestin-only injectable contraceptives.
Noristerat (Norethisterone enanthate): Another progestin-only option used in several countries.

Mechanism
Prevention of Ovulation: The injected progestin suppresses the secretion of FSH and LH, preventing the maturation and release of the egg from the ovary.
Thickening of Cervical Mucus: Progestin increases the viscosity of cervical mucus, forming a barrier that makes it difficult for sperm to reach the egg.
Endometrial Alteration: The endometrial lining becomes thin and less receptive to implantation, further preventing pregnancy.
Duration of Action:
A single intramuscular or subcutaneous injection provides contraceptive protection for approximately 3 months, after which a repeat dose is required for continued efficacy.
Advantages:
- High Effectiveness: When administered correctly, injectable contraceptives have a failure rate of less than 1%.
- Convenience: No daily dosing is required, making them suitable for women who may have difficulty remembering daily pills.
- Menstrual Benefits: Can reduce menstrual pain (dysmenorrhea) and lower the risk of anemia by decreasing menstrual blood loss.
- Discreet Use: Injectable contraceptives can be used without partners knowing, providing privacy in family planning.
Disadvantages / Side Effects:
- Menstrual Irregularities: Some women may experience irregular bleeding, spotting, or absence of periods (amenorrhea).
- Delayed Fertility Return: Fertility may take several months (sometimes up to 10 months) to return after discontinuation.
- Other Side Effects: Possible weight gain, headaches, mood changes, or bone mineral density reduction with long-term use.
- No Protection Against STIs: Injectable contraceptives do not protect against sexually transmitted infections, so additional barrier methods may be necessary.
c) Implants
Examples: Norplant, Implanon, Nexplanon.
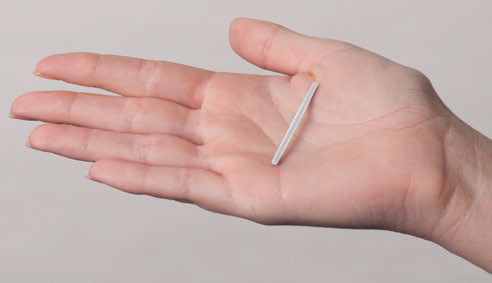
Description: Small, flexible rods implanted subdermally in the upper arm.
Mechanism: Slowly release progestin to inhibit ovulation.
Duration: 3–5 years.
Advantages: Long-acting, reversible, and safe.
Disadvantages: Irregular bleeding or spotting may occur initially.
d) Transdermal Patches and Vaginal Rings
Examples: Evra patch, NuvaRing.
Mechanism: Release estrogen and progestin through the skin or vaginal mucosa, inhibiting ovulation.
Advantages: Avoids gastrointestinal absorption; convenient.
Disadvantages: Local irritation or hormonal side effects.
4. Permanent (Surgical) Methods
These are irreversible procedures designed for individuals or couples who have completed their families and wish to prevent further pregnancies.
a) Vasectomy (Male Sterilization)
Procedure: Vasectomy is a minor surgical procedure that involves cutting and sealing the vas deferens—the tubes that carry sperm from the testes to the urethra.It is usually performed under local anesthesia in an outpatient setting, and the procedure typically takes 15–30 minutes.
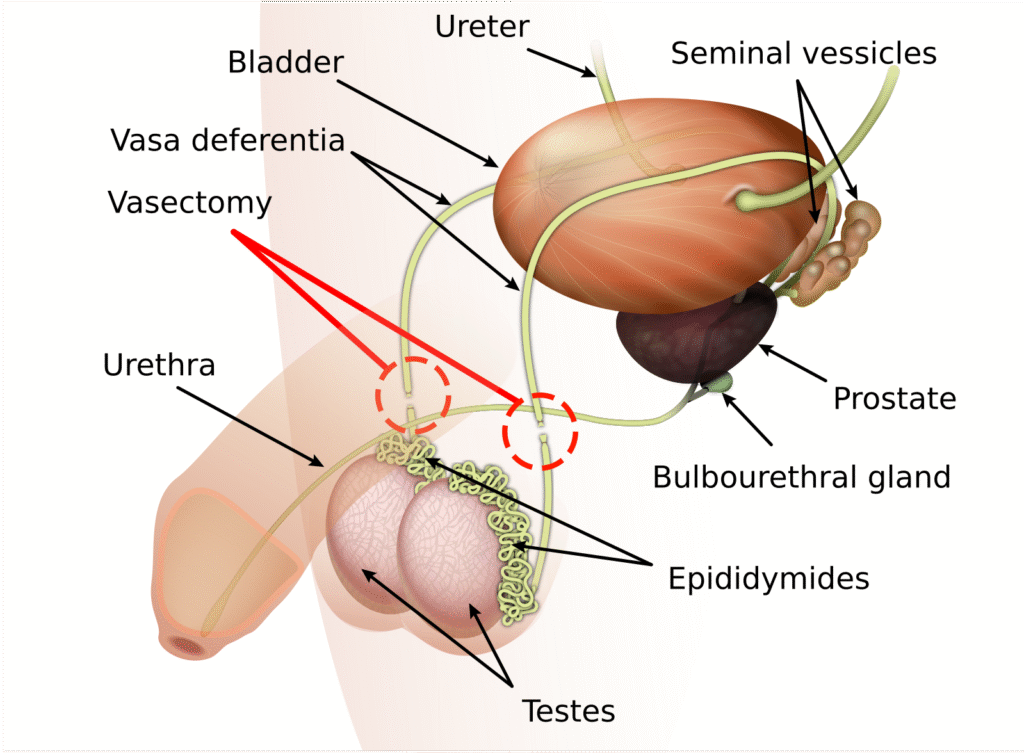
There are two main techniques: conventional incision method and no-scalpel vasectomy, with the latter associated with less pain and quicker recovery.
Effect on Fertility and Function:
- After vasectomy, sperm are prevented from entering the semen, making the man infertile.
- Sexual function, libido, testosterone levels, and ejaculatory volume remain largely unaffected.
- Fertility is not immediately zero; sperm clearance may take several weeks or ejaculations, so follow-up testing is required to confirm sterility.
Advantages:
- Simple and Safe: It is a relatively quick outpatient procedure with minimal complications.
- Highly Effective: Vasectomy has a very low failure rate (<1%) in preventing pregnancy.
- Permanent Solution: Offers a lifelong contraceptive option for men who are sure they do not want more children.
- No Hormonal Effects: Unlike female contraceptives, it does not affect hormonal balance or sexual function.
Disadvantages / Considerations:
- Reversibility Issues: Surgical reversal (vasovasostomy) is possible but complex, expensive, and not always successful.
- No STI Protection: Vasectomy does not protect against sexually transmitted infections, so barrier methods are still needed for STI prevention.
- Post-Procedure Risks: May include minor pain, swelling, hematoma, or infection at the surgical site.
- Psychological Considerations: Irreversibility may cause anxiety in some men, so thorough counseling is essential.
b) Tubectomy or Tubal Ligation (Female Sterilization)
Procedure: Tubectomy, also known as tubal ligation, is a surgical method of female sterilization in which the fallopian tubes are blocked, cut, tied, or sealed to prevent the egg from traveling from the ovaries to the uterus.
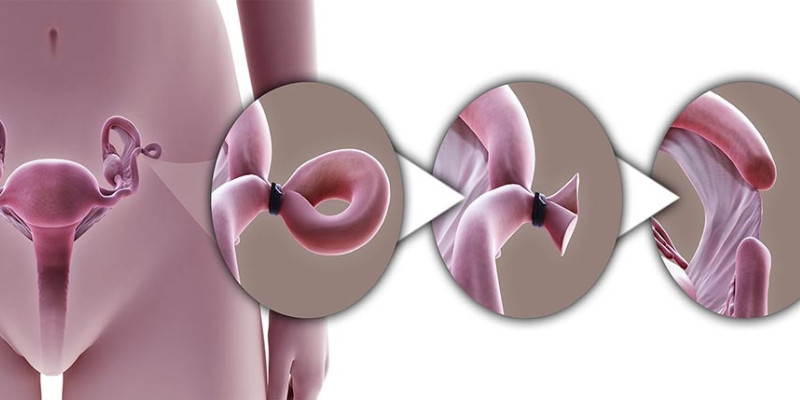
The procedure can be performed using different approaches:
- Laparoscopy: A minimally invasive technique using small abdominal incisions and a camera.
- Mini-laparotomy: A small abdominal incision, often used immediately after childbirth.
- Hysteroscopic sterilization: A non-incisional method where devices are inserted via the cervix to block the tubes (e.g., Essure, though less common now).
Typically done under general or local anesthesia, depending on the method and patient condition.
Effect on Fertility and Function:
- Tubectomy prevents the egg and sperm from meeting, effectively stopping fertilization.
- Since the ovaries continue to function normally, hormonal balance, menstrual cycles, and sexual function remain unaffected.
Advantages:
- Permanent Contraception: Highly effective and considered a lifelong solution for women who do not desire future pregnancies.
- No Hormonal Interference: Unlike hormonal contraceptives, it does not affect estrogen or progesterone levels.
- Convenience: Once performed, there is no need for ongoing contraception or compliance with pills or devices.
- Reduces Pregnancy-Related Risks: Particularly useful for women with high-risk pregnancies or those who have completed their families.
Disadvantages / Considerations:
- Surgical Risks: Requires anesthesia and surgery, which carries risks such as infection, bleeding, or injury to surrounding organs.
- Irreversibility: While reversal is sometimes possible, it is complex, expensive, and not always successful.
- Postoperative Complications: May include pain, adhesions, or rarely, ectopic pregnancy if the procedure fails.
- No STI Protection: Like male sterilization, tubectomy does not protect against sexually transmitted infections.
5. Emergency Contraceptive Devices
Emergency contraception is used after unprotected sexual intercourse or contraceptive failure to prevent pregnancy.
a) Emergency Contraceptive Pills
- Levonorgestrel-based pills (e.g., Plan B, i-Pill) – usually taken as a single dose or two doses 12 hours apart.
- Ulipristal acetate – a selective progesterone receptor modulator, more effective than levonorgestrel when taken closer to ovulation.
Mechanism of Action:
- Prevention or Delay of Ovulation: ECPs work primarily by inhibiting or delaying the release of an egg from the ovary, preventing fertilization.
- Alteration of Endometrial Lining: They may modify the uterine lining, making it less receptive to implantation of a fertilized egg.
- Effect on Cervical Mucus: In some cases, ECPs can also thicken cervical mucus, reducing the chance of sperm reaching the egg.
Timeframe for Effectiveness:
Most effective when taken as soon as possible after unprotected intercourse.
- Levonorgestrel: Effective up to 72 hours after intercourse, with decreasing effectiveness over time.
- Ulipristal acetate: Can be effective up to 120 hours (5 days) post-intercourse.
b) Copper IUD (Post-Coital Use)
- Mechanism: Copper ions are toxic to sperm and ova; prevent fertilization and implantation if inserted within 5 days.
- Advantages: Most effective emergency contraceptive method.
Advantages:
- Provides a backup method when regular contraception fails or is not used.
- Can help prevent unintended pregnancies without requiring medical procedures.
Disadvantages / Considerations:
- Not for Routine Use: ECPs are designed for emergency situations, not as a primary contraceptive method.
- Side Effects: May include nausea, fatigue, headache, dizziness, breast tenderness, or temporary changes in menstrual cycle timing.
- No STI Protection: ECPs do not prevent sexually transmitted infections.
- Effectiveness Limitation: Effectiveness decreases with increasing time after intercourse or in women with higher body weight (for levonorgestrel).
Characteristics of an Ideal Contraceptive Device
An ideal contraceptive device should:
- Be safe, effective, and reversible.
- Be easy to use and culturally acceptable.
- Have minimal side effects.
- Be economical and accessible.
- Not interfere with libido or sexual pleasure.
- Provide, if possible, protection against STIs.
Conclusion
Contraceptive devices represent one of the most significant achievements in the field of preventive medicine and reproductive health. They not only allow for the prevention of unwanted pregnancies but also support responsible parenthood, maternal health, and socioeconomic stability.
With advances in medical science, modern contraceptive devices are becoming increasingly safe, effective, and user-friendly. However, education, counseling, and proper medical guidance remain essential to ensure their correct and consistent use. The choice of a contraceptive method should always be individualized, taking into account health status, age, frequency of sexual activity, and personal preferences.
In essence, contraceptive devices serve as tools of empowerment, autonomy, and reproductive freedom, promoting not only personal well-being but also contributing to the broader goals of public health and population sustainability.

