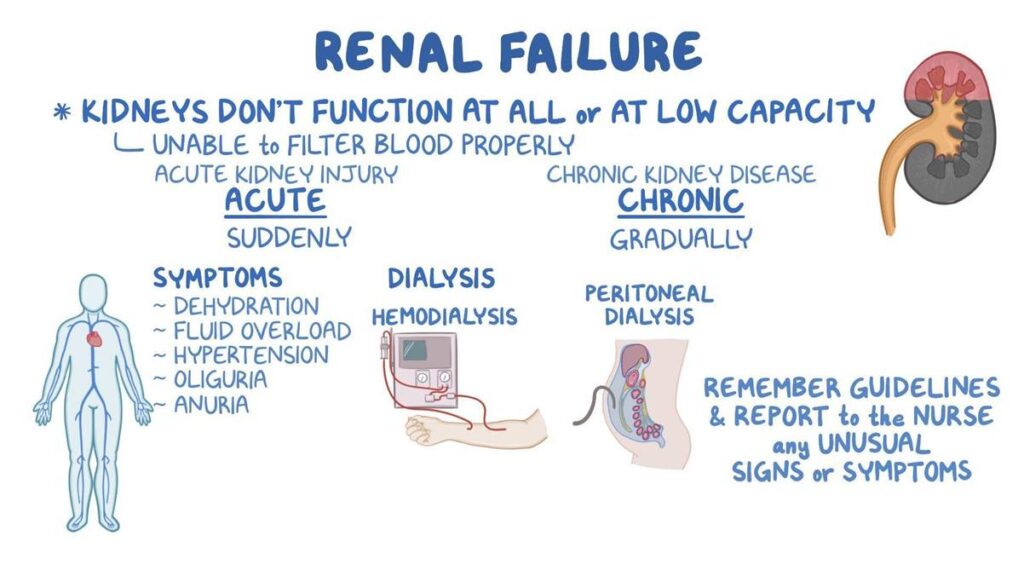
Renal failure, also known as kidney failure, occurs when the kidneys lose their ability to filter waste and excess fluids from the blood. This can lead to the accumulation of harmful substances in the body and disrupt the balance of electrolytes. Renal failure can be classified into two main types: acute renal failure (ARF) and chronic renal failure (CRF). This note explores the causes, pathophysiology, symptoms, diagnosis, treatment, and prevention of both acute and chronic renal failure.
Acute Renal Failure (Acute Kidney Injury)
Acute renal failure, now commonly referred to as acute kidney injury (AKI), is characterized by a sudden and often reversible loss of kidney function. It develops rapidly over a few hours or days and is typically identified by a rapid increase in serum creatinine levels or a decrease in urine output.
Step 1: Sudden Decline in Kidney Function
Acute renal failure begins with a sudden and rapid decrease in kidney function, occurring over hours to days. This can be triggered by various causes like severe dehydration, infection (sepsis), toxic drugs, or obstruction of urinary outflow. The kidneys fail to maintain their ability to filter waste products, balance electrolytes, and regulate fluid volume, resulting in the rapid accumulation of waste like urea and creatinine in the blood.
Step 2: Classification of AKI – Prerenal, Intrinsic, Postrenal
AKI is classified based on where the problem starts:
- Prerenal AKI occurs due to reduced blood flow to the kidneys, such as in shock, heart failure, or severe blood loss. The kidneys themselves are not damaged at first.
- Intrinsic AKI involves direct damage to kidney tissues, often from toxins, drugs (e.g., aminoglycosides), or conditions like acute tubular necrosis (ATN).
- Postrenal AKI is caused by obstruction in the urinary tract, such as from kidney stones, tumors, or prostate enlargement, which blocks urine flow and increases backpressure.
Step 3: Tubular Injury and Cell Death
In intrinsic AKI, especially inacute tubular necrosis, the cells lining the renal tubules become injured or die due to toxins or prolonged ischemia (lack of oxygen). Damaged cells slough off into the tubule lumen and form casts, which block the nephron. This leads to reduced glomerular filtration and contributes to further buildup of toxins and fluids in the body.
Step 4: Electrolyte Imbalance and Fluid Retention
As kidney function drops, the body retains sodium and water, leading to edema and hypertension. Simultaneously, the kidney fails to excrete potassium, leading to hyperkalemia, which can cause dangerous cardiac arrhythmias. The acid-base balance is also disrupted, resulting in metabolic acidosis, where the blood becomes too acidic.
Step 5: Potential Recovery or Progression
With prompt treatment of the underlying cause, AKI may be reversible, and kidney function can return to normal or near-normal levels. However, if the injury is severe or prolonged, it may lead to permanent nephron damage, potentially progressing to chronic kidney disease (CKD).
Chronic Renal Failure (Chronic Kidney Disease)
Chronic renal failure, now commonly referred to as chronic kidney disease (CKD), is characterized by a gradual and irreversible loss of kidney function over months or years. CKD is defined by a decrease in GFR or evidence of kidney damage (e.g., proteinuria) for at least three months.
Step 1: Gradual Nephron Loss
Chronic kidney disease develops slowly over months or years, often due to long-standing conditions like diabetes, hypertension, or chronic glomerulonephritis. These conditions cause ongoing injury to nephrons—the functional units of the kidneys. As more nephrons are damaged and lost, the remaining nephrons compensate by hyperfiltration, which eventually also damages them.
Step 2: Reduced Glomerular Filtration Rate (GFR)
As the number of functioning nephrons decreases, the glomerular filtration rate (GFR) gradually falls. When the GFR drops below 60 mL/min for more than 3 months, the condition is defined as CKD. Reduced GFR means less filtering of blood, leading to accumulation of waste products, fluid overload, and electrolyte imbalances.
Step 3: Azotemia and Uremia
With declining GFR, waste products like urea, creatinine, and ammonia accumulate in the blood—a condition called azotemia. When these toxins begin to cause symptoms like fatigue, nausea, confusion, and pericarditis, it progresses to uremia, which is a severe and life-threatening stage of CKD.
Step 4: Electrolyte and Acid-Base Disturbances
CKD results in multiple imbalances:
- Hyperkalemia due to reduced potassium excretion
- Hyperphosphatemia and hypocalcemia, contributing to bone disease (renal osteodystrophy)
- Metabolic acidosis due to failure to excrete hydrogen ions
These contribute to symptoms like bone pain, muscle weakness, arrhythmias, and poor growth in children.
Step 5: Anemia and Hormonal Distrubance
The kidneys produceerythropoietin, which stimulates red blood cell production. In CKD, the production drops, leading tonormocytic, normochromic anemia. Also, activation of vitamin Dis impaired, which reduces calcium absorption and contributes to bone disease. Therenin-angiotensin-aldosterone system (RAAS)may also become overactive, worseninghypertension.
Step 6: End-Stage Renal Disease (ESRD)
When GFR falls below 15 mL/min/1.73 m², the kidneys can no longer maintain basic functions. This stage is called end-stage renal disease, requiring dialysis or kidney transplantation to sustain life. Without intervention, ESRD leads to severe fluid overload, electrolyte imbalances, uremia, and ultimately death.
Conclusion
Acute and chronic renal failure represent significant health challenges with serious implications for affected individuals. Understanding the causes, pathophysiology, symptoms, diagnosis, treatment, and prevention of both acute and chronic renal failure is essential for effective management and improving patient outcomes. Early detection, appropriate medical interventions, and lifestyle modifications can help prevent progression and mitigate complications associated with renal failure.

