The human nervous system includes 12 pairs of cranial nerves, each emerging directly from the brain rather than the spinal cord. These nerves play critical roles in sensory perception, motor control, and autonomic regulation in the head, neck, and thoracic-abdominal regions. Understanding the anatomy and function of each cranial nerve is crucial for neurological assessment, diagnosis, and clinical intervention.
1. Olfactory Nerve (Cranial Nerve I)
- Primary Function: Responsible for the sense of smell (olfaction).
- Anatomical Pathway: Olfactory nerve fibers originate from the olfactory receptor neurons in the nasal epithelium. These axons pass through the cribriform plate of the ethmoid bone to synapse in the olfactory bulbs, which relay information to the olfactory cortex in the temporal lobe.
- Clinical Significance: Damage may lead to anosmia (loss of smell), affecting taste perception and potentially signaling neurodegenerative disorders such as Parkinson’s or Alzheimer’s disease.
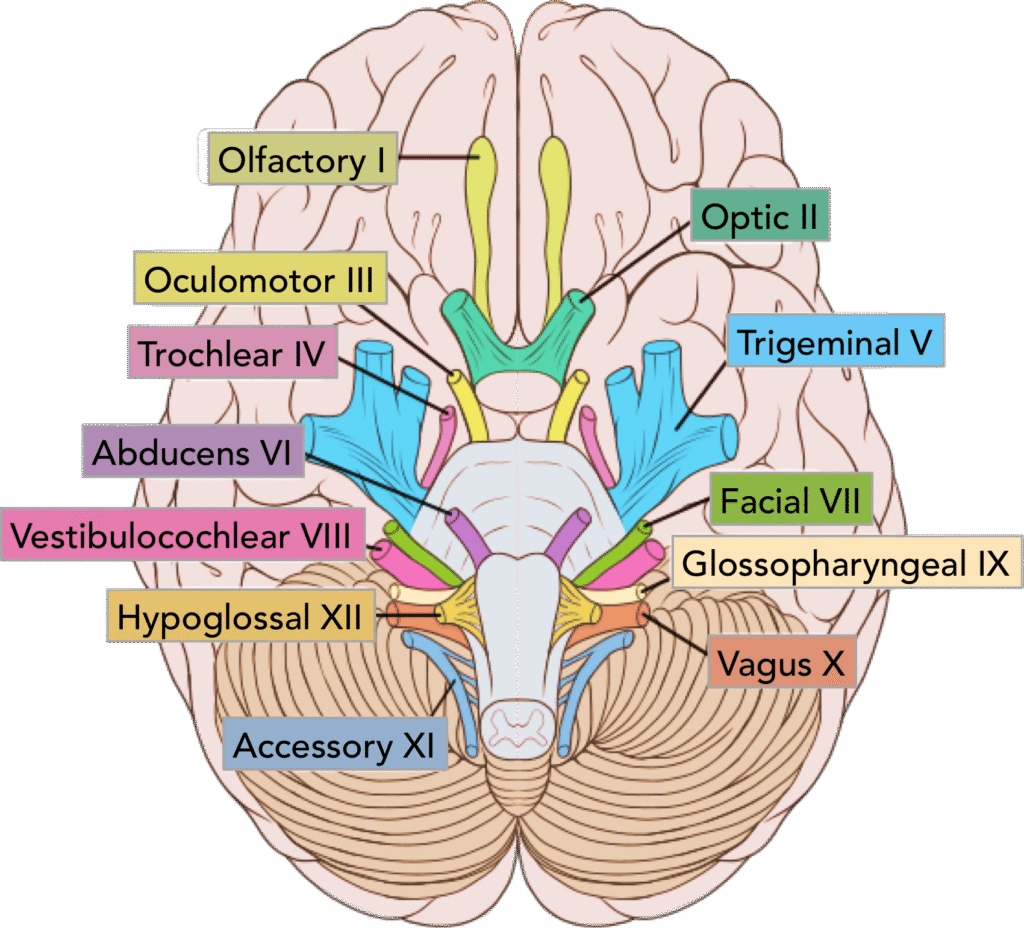
2. Optic Nerve (Cranial Nerve II)
- Primary Function: Responsible for vision, transmitting visual information from the retina to the brain.
- Anatomical Pathway: Retinal ganglion cell axons form the optic nerve, which converges at the optic chiasma, where fibers partially decussate, and then project via the optic tracts to the lateral geniculate nucleus of the thalamus and onward to the primary visual cortex in the occipital lobe.
- Clinical Significance: Lesions can cause visual field defects, blindness, or optic neuritis, often observed in conditions like multiple sclerosis.
3. Oculomotor Nerve (Cranial Nerve III)
- Primary Function: Controls most eye movements, including eyelid elevation, pupillary constriction, and lens accommodation for near vision.
- Anatomical Pathway: Emerges from the midbrain and innervates four of the six extraocular muscles: superior, inferior, and medial rectus, and inferior oblique, as well as the levator palpebrae superioris. Parasympathetic fibers control pupillary constrictor and ciliary muscles.
- Clinical Significance: Lesions may cause ptosis (drooping eyelid), diplopia (double vision), and pupillary dilation, often seen in cranial nerve palsies or compressive lesions.
4. Trochlear Nerve (Cranial Nerve IV)
- Primary Function: Innervates the superior oblique muscle, enabling the eye to look downward and inward.
- Anatomical Pathway: Originates from the dorsal midbrain, the only cranial nerve to emerge dorsally and to cross completely before exiting the brainstem.
- Clinical Significance: Damage results in vertical diplopia, difficulty reading or descending stairs, and compensatory head tilt.
5. Trigeminal Nerve (Cranial Nerve V)
- Primary Function: Responsible for facial sensation (touch, pain, temperature) and mastication (chewing).
- Anatomical Pathway: Three major branches:
- Ophthalmic (V1): Sensory innervation of the forehead, scalp, and eye.
- Maxillary (V2): Sensory innervation of the midface, upper teeth, and nasal cavity.
- Mandibular (V3): Sensory innervation of lower face and motor fibers for chewing muscles.
- Clinical Significance: Lesions can cause trigeminal neuralgia, severe facial pain, or loss of facial sensation, significantly impacting quality of life.
6. Abducent Nerve (Cranial Nerve VI)
- Primary Function: Controls the lateral rectus muscle, which abducts the eye (moves it outward).
- Anatomical Pathway: Arises from the pons and travels to the orbit via the superior orbital fissure.
- Clinical Significance: Lesions lead to medial deviation of the eye (strabismus) and horizontal diplopia, especially when attempting lateral gaze.
7. Facial Nerve (Cranial Nerve VII)
- Primary Function: Controls facial expressions, taste sensation on the anterior two-thirds of the tongue, and secretion of salivary and lacrimal glands.
- Anatomical Pathway: Emerges from the pons, traverses the internal acoustic meatus, and branches extensively to innervate facial muscles.
- Clinical Significance: Damage may cause Bell’s palsy, characterized by facial drooping, inability to close the eye, loss of taste, and reduced salivation.
8. Vestibulocochlear Nerve (Cranial Nerve VIII)
- Primary Function: Responsible for hearing (cochlear division) and balance and equilibrium (vestibular division).
- Anatomical Pathway: Fibers from the cochlea and vestibular apparatus converge to form the nerve, which projects to the brainstem nuclei for auditory processing and balance integration.
- Clinical Significance: Lesions may cause hearing loss, vertigo, nystagmus, or balance disturbances, as observed in vestibular neuritis or acoustic neuroma.
9. Glossopharyngeal Nerve (Cranial Nerve IX)
- Primary Function: Controls taste and sensation in the posterior one-third of the tongue, swallowing muscles, and contributes to salivary gland secretion.
- Anatomical Pathway: Emerges from the medulla oblongata, innervating the pharynx, carotid body, and posterior tongue.
- Clinical Significance: Lesions may lead to loss of gag reflex, impaired swallowing, and taste disturbances.
10. Vagus Nerve (Cranial Nerve X)
- Primary Function: A mixed nerve regulating involuntary functions of the heart, lungs, and digestive tract.
- Anatomical Pathway: Emerges from the medulla, extending to thoracic and abdominal organs, providing parasympathetic innervation.
- Clinical Significance: Damage may result in voice changes (dysphonia), swallowing difficulties, abnormal heart rate, or digestive disturbances.
11. Accessory Nerve (Cranial Nerve XI)
- Primary Function: Controls neck and shoulder muscles, including the sternocleidomastoid and trapezius, allowing head rotation, flexion, and shoulder elevation.
- Anatomical Pathway: Has both cranial and spinal roots, with spinal fibers ascending into the cranial cavity and exiting through the jugular foramen.
- Clinical Significance: Lesions cause weakness in shoulder elevation, difficulty turning the head, and muscle atrophy.
12. Hypoglossal Nerve (Cranial Nerve XII)
- Primary Function: Controls tongue movements, essential for speech, swallowing, and food manipulation.
- Anatomical Pathway: Originates from the medulla, exiting the skull via the hypoglossal canal, and innervates intrinsic and extrinsic tongue muscles.
- Clinical Significance: Damage leads to tongue deviation toward the affected side, atrophy, and difficulties with articulation and swallowing.
Functional Overview and Clinical Relevance
Cranial nerves perform a diverse range of sensory, motor, and autonomic functions, allowing precise coordination of vision, hearing, taste, smell, facial expression, eye movements, and vital organ regulation. Comprehensive understanding of these nerves is essential for neurological assessment, diagnosis of cranial nerve palsies, and management of sensory or motor deficits. Clinicians routinely test cranial nerve function to detect early signs of neurological diseases, tumors, or trauma.
Summary Table of Cranial Nerves
| Cranial Nerve | Function | Key Clinical Relevance |
|---|---|---|
| I – Olfactory | Smell | Anosmia |
| II – Optic | Vision | Blindness, visual field defects |
| III – Oculomotor | Eye movements, pupil constriction | Ptosis, diplopia |
| IV – Trochlear | Superior oblique muscle | Vertical diplopia |
| V – Trigeminal | Facial sensation, mastication | Trigeminal neuralgia |
| VI – Abducent | Lateral rectus muscle | Medial strabismus |
| VII – Facial | Facial expression, taste, salivation | Bell’s palsy |
| VIII – Vestibulocochlear | Hearing, balance | Vertigo, hearing loss |
| IX – Glossopharyngeal | Taste (posterior tongue), swallowing | Dysphagia, taste loss |
| X – Vagus | Parasympathetic control of thoracoabdominal organs | Dysphonia, autonomic dysfunction |
| XI – Accessory | Neck and shoulder muscles | Weakness turning head, shoulder drop |
| XII – Hypoglossal | Tongue movements | Tongue deviation, dysarthri |