Gonorrhea
Gonorrhea is a highly prevalent sexually transmitted infection (STI) caused by the pathogenic bacterium Neisseria gonorrhoeae. It represents one of the most significant bacterial STIs globally and remains a major challenge to public health systems due to its high transmission rate, frequent asymptomatic nature, severe reproductive complications, and the alarming emergence of multidrug-resistant strains. The infection primarily targets mucosal surfaces lined by columnar epithelium, particularly within the urogenital tract, but it may also affect extragenital sites such as the rectum, pharynx, conjunctiva, and, in advanced cases, disseminate systemically.
A defining feature of gonorrhea is that a substantial proportion of infected individuals—especially women—remain asymptomatic or minimally symptomatic, allowing the infection to persist undetected and facilitating ongoing transmission within the community.
Etiopathogenesis
1. Causative Agent
Neisseria gonorrhoeae is a Gram-negative, non-motile, non-spore-forming diplococcus, characteristically arranged as kidney- or coffee bean–shaped pairs. The organism is an obligate human pathogen with no known animal reservoir. It possesses several virulence determinants that enable colonization, immune evasion, and tissue damage, including:
- Type IV pili, which mediate attachment to epithelial cells and undergo antigenic variation
- Outer membrane proteins (Por proteins) that interfere with host immune responses
- Lipooligosaccharides (LOS), which trigger intense inflammatory reactions
- IgA protease, which degrades mucosal immunoglobulins
These virulence factors collectively contribute to persistent infection, inflammation, and tissue injury.
2. Mode of Transmission
Gonorrhea is transmitted predominantly through unprotected sexual contact, including vaginal, anal, and oral intercourse. The bacterium spreads efficiently through exposure to infected mucosal secretions. Vertical transmission from mother to neonate may occur during passage through an infected birth canal, resulting in neonatal ocular infection.
3. Site of Infection
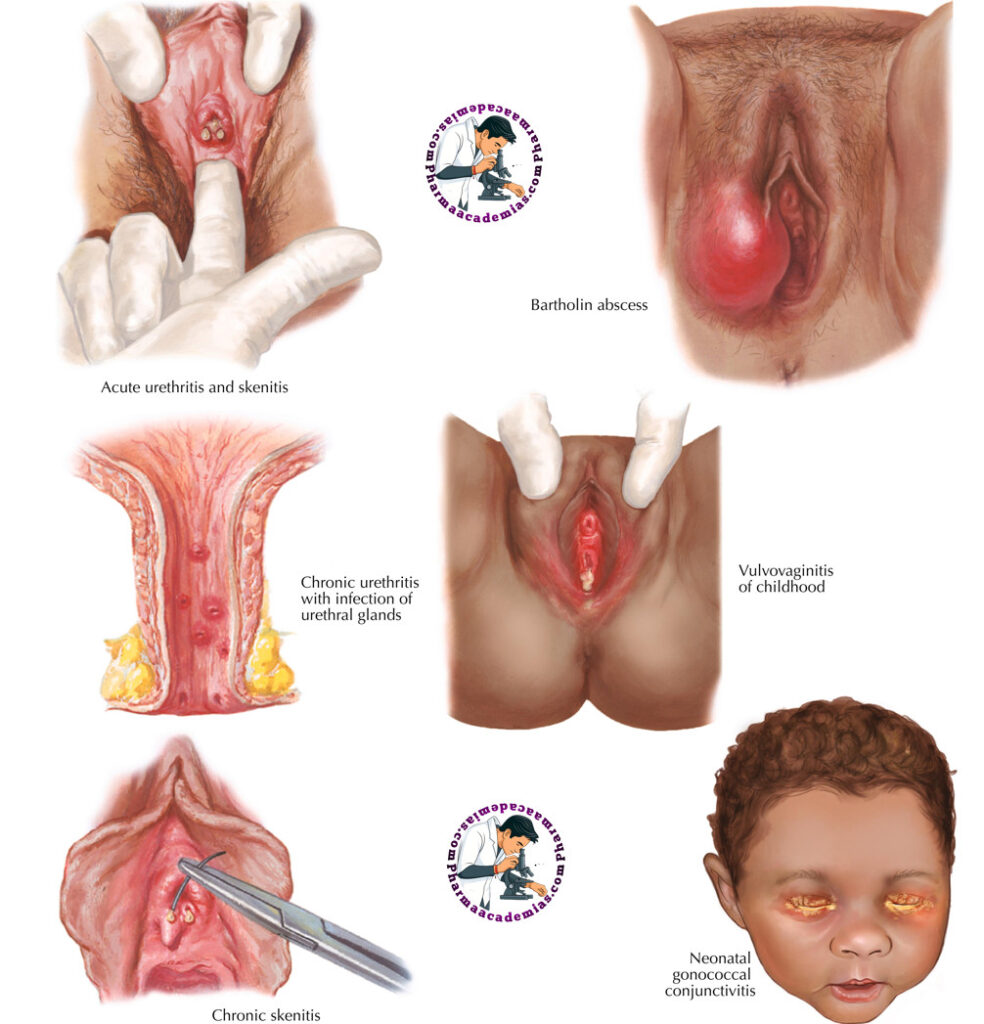
The organism preferentially infects columnar and transitional epithelium, commonly involving:
- Urethra (both sexes)
- Endocervix (women)
- Rectum (especially in individuals engaging in receptive anal intercourse)
- Pharynx (oral sexual exposure)
- Conjunctiva (newborns and rarely adults)
Squamous epithelium is relatively resistant, explaining why vaginal involvement is less prominent compared to the cervix.
4. Incubation Period
The incubation period typically ranges from 2 to 14 days, though symptoms may appear earlier in men. In women, infection often remains subclinical for extended periods.
Pathogenesis
Following exposure, N. gonorrhoeae adheres to epithelial cells using pili and surface adhesins. The organism then penetrates the mucosal barrier, multiplying within epithelial cells and subepithelial tissues. This invasion elicits a robust neutrophilic inflammatory response, leading to the characteristic purulent discharge. Despite this immune activation, antigenic variation and immune evasion mechanisms allow the bacterium to persist and spread locally or systemically.
Clinical Manifestations
1. Urethral Gonorrhea (Predominantly in Men)
Urethral infection in men is usually acute and symptomatic, presenting with:
- Dysuria and burning micturition
- Profuse purulent or mucopurulent urethral discharge
- Urinary frequency and urgency
If left untreated, the infection may extend to adjacent structures, resulting in:
- Epididymitis
- Orchitis
- Prostatitis
These complications can impair fertility.
2. Cervical Gonorrhea (Predominantly in Women)
Cervical infection is frequently asymptomatic, earning gonorrhea the reputation of a “silent infection” in women. When present, symptoms may include:
- Increased or abnormal vaginal discharge
- Intermenstrual or postcoital bleeding
- Dysuria
- Lower abdominal or pelvic discomfort
Delayed diagnosis significantly increases the risk of ascending infection.
3. Rectal Gonorrhea
Rectal infection may be asymptomatic or cause:
- Anal pain and itching
- Mucopurulent rectal discharge
- Tenesmus
- Rectal bleeding
4. Pharyngeal Gonorrhea
Pharyngeal infection is usually asymptomatic or mildly symptomatic, presenting with:
- Sore throat
- Pharyngeal erythema
This site is clinically important due to its role in antimicrobial resistance development.
Complications
1. Disseminated Gonococcal Infection (DGI)
Hematogenous spread of the organism can result in disseminated gonococcal infection, characterized by:
- Fever and malaise
- Migratory polyarthritis
- Tenosynovitis
- Pustular or necrotic skin lesions
In rare cases, DGI may progress to endocarditis, meningitis, or septic arthritis, conditions associated with significant morbidity and mortality.
2. Pelvic Inflammatory Disease (PID)
In women, untreated gonorrhea can ascend to involve the uterus, fallopian tubes, and ovaries, leading to PID. Long-term consequences include:
- Chronic pelvic pain
- Tubal scarring
- Infertility
- Increased risk of ectopic pregnancy
3. Neonatal Gonococcal Infection
Neonates exposed during childbirth may develop ophthalmia neonatorum, presenting with severe conjunctivitis, corneal ulceration, and potential blindness if untreated.
Diagnostic Evaluation
1. Culture
Culture remains important for:
- Confirmatory diagnosis
- Monitoring antimicrobial resistance
Specimens are obtained from urethral, cervical, rectal, or pharyngeal sites.
2. Nucleic Acid Amplification Tests (NAATs)
NAATs are the diagnostic gold standard, offering:
- High sensitivity and specificity
- Ability to test non-invasive specimens such as urine
- Detection of asymptomatic infections
3. Gram Stain
In symptomatic men, Gram stain demonstrating intracellular Gram-negative diplococci is highly suggestive. However, sensitivity is lower in women and extragenital infections.
Non-Pharmacological Management
1. Preventive Strategies
Effective prevention includes:
- Consistent condom use
- Sexual health education
- Regular STI screening, particularly in high-risk populations
2. Partner Management
Partner notification and treatment are essential to prevent reinfection and onward transmission.
3. Behavioral Interventions
Temporary sexual abstinence is advised until treatment completion and symptom resolution.
Pharmacological Management
1. Antibiotic Therapy
Current treatment guidelines recommend dual antibiotic therapy, typically:
- Ceftriaxone (intramuscular)
- Azithromycin (oral)
This regimen addresses co-infection with Chlamydia trachomatis and helps curb resistance development.
2. Follow-Up and Test of Cure
Follow-up testing is recommended in:
- Pharyngeal infections
- Suspected treatment failure
- High-risk individuals
3. Partner Treatment
All recent sexual partners should receive empirical treatment.
Public Health Measures
1. Surveillance and Contact Tracing
Robust surveillance systems help track infection trends and resistance patterns.
2. Health Education and Awareness
Public health campaigns emphasize:
- Safe sexual practices
- Early diagnosis
- Importance of treatment adherence
3. Vaccination Status
Although no specific gonorrhea vaccine exists, immunization against other STIs contributes to comprehensive sexual health strategies.
Conclusion
Gonorrhea is a clinically significant, globally prevalent STI with the potential for severe reproductive and systemic complications. The asymptomatic nature of many infections, combined with rising antimicrobial resistance, underscores the need for early diagnosis, effective treatment, partner management, and strong public health interventions. Sustained efforts in education, screening, and surveillance are essential to reduce the disease burden and prevent long-term sequelae.

