Introduction
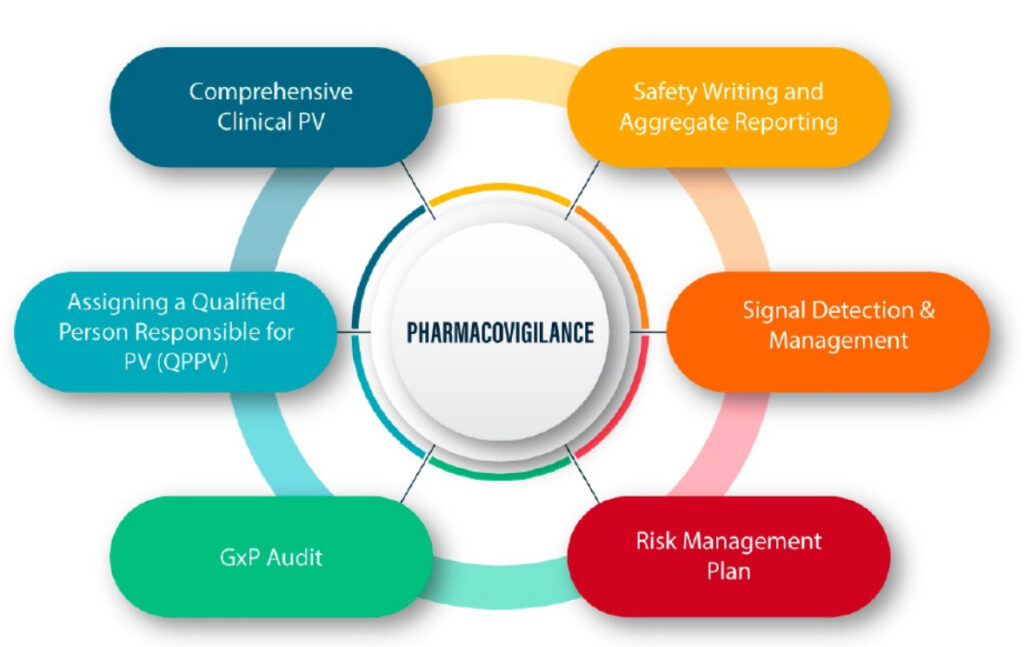
Pharmacovigilance (PV) is the science dedicated to detecting, assessing, understanding, and preventing adverse effects or any other drug-related problems. At its core, pharmacovigilance relies on robust communication pathways to ensure that safety data flows efficiently from source to stakeholder. Whether it’s sharing case reports with regulatory agencies, briefing business partners on risk management strategies, counseling healthcare facilities on reporting processes, or engaging media to inform the public, clear and timely communication is pivotal. Effective communication is not merely the act of sending and receiving information; it encompasses the quality, transparency, and mutual understanding necessary to make informed decisions that ultimately protect patient health and uphold public trust. This document delves into the principles and best practices for effective communication across various facets of pharmacovigilance.
1. Effective Communication in Pharmacovigilance
- Principles of Clear Messaging
- Accuracy & Clarity: Communication in PV must use precise, scientific terminology while remaining accessible to the intended audience. Misinterpretation of terms such as “serious” vs. “severe” adverse events can lead to major clinical and regulatory consequences. Clarity avoids miscommunication that could compromise safety.
- Consistency: Harmonizing language and content across documents, reports, and stakeholder communications ensures that all parties receive a uniform message. Discrepancies between internal and external communications can lead to confusion, delays, or loss of credibility.
- Timeliness: Prompt communication of emerging safety issues is essential to prevent harm. Delays in transmitting information—whether due to internal bottlenecks or unclear procedures—can put patient safety at risk.
- Audience-Centric Language: It is crucial to adapt the complexity of the message to the audience. Regulatory authorities may require data-rich submissions, while healthcare professionals need clinically actionable guidance. Laypersons and patients require plain-language explanations.
- Channels & Tools
- Electronic Databases & Portals: These include systems like EudraVigilance, FAERS (FDA Adverse Event Reporting System), and VigiBase, which allow secure and standardized transmission of safety data. The ICH E2B(R3) format ensures global compatibility.
- Internal Dashboards: These are used by PV teams to monitor real-time data on adverse event trends, product performance, and potential signals that require further evaluation.
- Standard Operating Procedures (SOPs): Clear, documented workflows help ensure consistent execution of safety communications. SOPs guide employees on how and when to escalate safety information.
- Workshops & Training: Ongoing education ensures all team members and collaborators understand reporting requirements, timelines, and how to use relevant tools. This helps maintain compliance and reduces errors.
- Documentation & Archiving
Communication in PV must be traceable. All exchanges—whether internal discussions, regulatory submissions, or external press releases—must be archived properly. This ensures accountability and provides a legal and regulatory record.
Version control prevents the dissemination of outdated or incorrect information, especially in rapidly evolving safety situations.
2. Communication in Drug Safety Crisis Management
A drug safety crisis is any event that threatens patient safety or company integrity, such as the detection of a new life-threatening adverse effect, contamination of a product batch, or a sudden surge in reported ADRs. In such high-stakes situations, communication must be swift, coordinated, and reassuring to all stakeholders.
- Crisis Communication Team (CCT)
Composition: A multidisciplinary team is essential. It should include pharmacovigilance experts (who understand the data), medical affairs (to assess clinical implications), regulatory affairs (to manage interactions with authorities), legal advisors (to ensure compliance), and public relations or communication specialists (to craft public messaging).
Roles & Responsibilities: Delegating responsibilities ensures no step is overlooked. For example, one team may draft the press release while another manages media inquiries, and yet another monitors public sentiment.
- Crisis Communication Plan
Pre-Crisis Preparedness: Organizations should conduct simulations to test their response systems. Templates for media responses, DHP letters, and FAQs should be developed in advance to save valuable time during a real crisis.
Activation Triggers: The plan should specify what types of events qualify as a crisis and how quickly the communication should begin. This prevents delays due to uncertainty.
- Key Messages & FAQs
These are prepared to ensure consistent, accurate, and empathetic messaging. They should explain what is known, what is being done, and what affected individuals should do.
- Stakeholder Notifications
Internal: Immediate communication to top leadership and frontline teams ensures everyone is aligned. This enables swift implementation of mitigation strategies.
External: Stakeholders such as HCPs, patients, and regulators must receive timely updates, with clear guidance on how to handle the issue (e.g., stopping drug use, monitoring for symptoms, etc.).
- Feedback & Monitoring
Monitoring social and mainstream media allows the organization to assess public perception and correct misinformation. A feedback loop ensures updates and follow-up actions are communicated as the situation evolves.
3. Communicating with Regulatory Agencies
Regulatory agencies are primary stakeholders in drug safety oversight. Communication with them must be proactive, transparent, and data-driven.
- Regulatory Submissions
Individual Case Safety Reports (ICSRs): These must include detailed clinical data, patient history, timelines, and suspected relationships to the drug. Errors or omissions can lead to regulatory findings.
PSURs/DSURs: These documents provide a cumulative analysis of all safety data, including signal detection, benefit-risk assessment, and proposed label changes. They must follow international formats and be submitted on schedule.
RMPs/REMS: These describe known risks, how they will be mitigated, and how the effectiveness of those measures will be evaluated. Communicating this information clearly ensures regulatory approval and market continuity.
- Meetings & Teleconferences
Preparation: Pre-submitting materials allows regulators to ask informed questions. Clear agendas prevent scope drift.
Conduct: Meetings should be documented thoroughly, with minutes and action items distributed promptly.
- Regulatory Inquiries & Deficiencies
Responses should be timely and comprehensive, backed by data and scientific rationale. Delayed or incomplete responses can affect approvals or lead to sanctions.
- Best Practices
Engage early with regulators when a new safety issue is identified. Preemptive communication shows accountability and fosters cooperation.
Acknowledge data gaps or uncertainties honestly, while also communicating planned actions to address them.
4. Communicating with Business Partners
In global drug development and commercialization, business partners such as CROs, licensees, and distributors are involved in safety data generation and management. Misalignment can lead to compliance breaches.
- Agreements & Contracts: PV agreements should clearly define roles, responsibilities, timelines for case reporting, formats, contact points, and audit rights. These help prevent disputes and ensure regulatory compliance. Escalation pathways must be clearly laid out for urgent safety concerns, such as suspected unexpected serious adverse reactions (SUSARs).
- Regular Reporting: Regularly shared safety dashboards keep all parties aware of trends, compliance rates, and signal detection results. Transparency strengthens trust and collaboration. Joint periodic reviews of cumulative safety data encourage proactive risk mitigation.
- Training & Audits: Training ensures that all partners are familiar with relevant regulations, SOPs, and reporting tools. Routine audits verify that partners meet data quality standards and reporting obligations.
5. Communicating with Healthcare Facilities
Healthcare professionals (HCPs) are often the first to observe ADRs. Their cooperation is vital to the success of any pharmacovigilance system.
- Education & Outreach: Educating HCPs about the importance of reporting ADRs and how to do so increases the quality and volume of data. CME sessions, brochures, and online modules are useful tools. Hospital-based roundtables encourage HCPs to share their experiences and learn from others, promoting a culture of safety.
- Reporting Tools: User-friendly apps and web-based portals simplify the reporting process. Intuitive interfaces, auto-fill options, and real-time acknowledgment make it more likely that HCPs will report. Paper forms should be accessible and accompanied by clear instructions and contact information.
- Feedback Loop: Acknowledging HCP contributions fosters engagement. Letting them know how their reports contributed to safety decisions builds motivation. Bulletins summarizing ADR trends, regulatory decisions, and case studies help close the loop and reinforce continuous learning.
6. Communicating with Media
The media, including news outlets and social platforms, can amplify both facts and misinformation. Strategic engagement is essential to maintain public trust.
- Media Relations Strategy: Designated spokespeople should be trained in risk communication, avoiding speculation and maintaining composure under pressure. Media kits should be prepared ahead of time, containing fact sheets, timelines, expert bios, and FAQs.
- Press Releases & Statements: Clear structure and empathetic tone are crucial. The message should lead with the key fact, explain context, and describe what is being done. Avoid technical jargon that can be misinterpreted by lay audiences.
- Digital & Social-Media: Visual aids such as infographics and video clips can simplify complex safety data. Q&A sessions on platforms like YouTube or LinkedIn provide transparency. Monitoring social media helps detect rumors or panic. Swift, factual responses prevent escalation.
- Crisis-Specific Communication: All communication during a crisis should align with the overall message strategy. Contradictory statements from different spokespeople can erode trust. Frequent updates are important, even if there is no new information. It demonstrates ongoing engagement and transparency.
Conclusion
Effective communication in pharmacovigilance transcends mere data exchange—it is the lifeline that connects patients, healthcare providers, regulators, business partners, and the public. It involves a coordinated strategy that ensures messages are accurate, consistent, timely, and tailored to the audience. By adhering to principles of clarity, transparency, empathy, and responsibility, organizations can not only meet regulatory requirements but also foster trust, protect patient safety, and enhance the reputation and resilience of their pharmacovigilance systems. In an increasingly connected world, where information travels fast, mastering the art and science of communication in PV is not optional—it is essential.

